Understanding the Difference between Types of Catastrophic Brain Injuries
 It’s easy to get lost in the language of the medical world. So much terminology goes into every condition and even then there’s usually more than one name for something. Those who aren’t intimately familiar with this field can find it commonplace to use certain conditions or terms interchangeably with little understanding of the intricate differences between them.
It’s easy to get lost in the language of the medical world. So much terminology goes into every condition and even then there’s usually more than one name for something. Those who aren’t intimately familiar with this field can find it commonplace to use certain conditions or terms interchangeably with little understanding of the intricate differences between them.
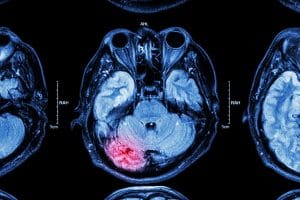
Catastrophic injuries are one of the areas where it can be simple to accidentally confuse one brain condition for another, but make no mistake, they can be very different. It’s important to understand the differences between causes, treatments, and prognoses when you or your loved one experiences a traumatic brain injury that places him or her into a coma, minimally conscious state, Persistent vegetative state, or they have brain death.
What is a coma?
Comas involve damage to parts of the brain such as the thalamus, brainstem, or both brain hemispheres. When a patient enters a coma, he or she can’t be awakened by outside factors such as touch or sound. A victim also won’t have a reaction to stimuli such as pain or other physical senses nor do they have sleep-wake cycles. There is no way to predict how long a patient may be in this state. It can be days or weeks, and if it lasts longer, your loved one has likely transitioned into what’s known as a persistent vegetative state, which is discussed below. Patients who fall into a coma due to severe brain damage may need assistance with breathing or be permanently disabled upon regaining consciousness.
This is not to be confused with a medically induced coma, which a patient can be brought out of by removing the drug that is keeping them in a coma-like state to allow time to heal from other wounds.
Causes of coma include:
- Traumatic brain injury
- Stroke
- Brain hemorrhage
- Severe hypothermia
- Drug overdose
- Drowning
- Cardiac arrest
- Diabetes
- Infection
Treatment often requires:
- Physical therapy
- Nursing care
- Medication to reduce brain swelling, infection or other underlying condition
What is a minimally conscious state?
This state allows patients to have some awareness of what’s happening around them, though it can be sporadic. Patients typically appear drowsy and unresponsive, but unlike with comas, they have the ability to respond to commands such as “squeeze my hand” or can mouth words. They can also react to pain stimuli and even hold objects.
It can be emotionally devastating to not be able to understand what your family member is experiencing because you can’t communicate with them, but they have the potential to improve in time but still may be left with a severe disability. These brain conditions can essentially be a step up process for victims who are able to recover. Even while some patients in a persistent vegetative state remain in one permanently, frequently they progress to being in a minimally conscious state that they can eventually surface from depending upon the cause of their brain injury and available care and treatments.
What is a persistent vegetative state?
As stated above, patients who begin in a coma may end up in a persistent vegetative state if the unconsciousness extends beyond a matter of weeks. Patients in this state have no awareness of their surroundings and lack the ability to understand commands or communicate.
Provided there isn’t any brainstem damage, a brain injury victim in this condition may be perfectly capable of breathing without assistance and will be able to:
- Open their eyes
- Experience sleep-wake cycles
- Grind their teeth
- Make sounds
- Make some physical movements
- Appear to make facial expressions
Causes generally include:
- Head trauma
- Brain damage
- Illness
- Stroke
What is brain death?
When a family member experiences brain death it means he or she no longer has any measurable brain activity due to a devastating injury to the brain and brainstem, or lack of oxygen to the brain long enough to cause permanent, irreversible damage. These patients have no ability to breathe on their own and will never be able to take a breath without mechanical assistance. It’s a harsh reality that can be difficult for families to accept, but a family member in this condition has no chance of even minor improvement or recovery. In clinical terms, your family member has died.
After suffering a catastrophic injury due to someone’s negligence, your loved one could come out of a coma quickly or may remain in a persistent vegetative state for decades depending upon the severity of the brain injury. You need to be able to focus on the parts of his or her care that you can control, such as payment of medical bills and securing necessary treatment should your family member regain consciousness.
Trying to manage everything alone can wreak havoc on your physical and financial health. You need help from the knowledgeable Mississippi traumatic brain injury attorneys at Merkel & Cocke, P.A. To schedule your free consultation, call 662-302-2979 or complete our contact form. We operate offices in Jackson, Clarksdale, and Oxford in addition to serving clients in the City of Tupelo.

Since 1982, Merkel & Cocke, P.A. has offered thorough, aggressive legal representation on behalf of clients throughout Mississippi. As one of the largest plaintiffs’ personal injury law firms in the state, we consider it our duty and our honor to serve the people of our communities, and to uphold their rights in court. Our reputation is such that other law firms turn to us when they need legal counsel, and our business has grown through the years because of the referrals of these attorneys, who trust us with their needs and the needs of their clients. We are the firm you can trust when there are challenges ahead. To schedule a free consultation, please complete our contact form.
